Editor’s note: The North American Pain School (NAPS) took place 19-24 June 2022, in Montebello, Québec City, Canada. NAPS – an educational initiative of the International Association for the Study of Pain (IASP) and Analgesic, Anesthetic, and Addiction Clinical Trial Translations, Innovations, Opportunities, and Networks (ACTTION), and presented by the Quebec Pain Research Network (QPRN) – brings together leading experts in pain research and management to provide trainees with scientific education, professional development, and networking experiences. This year’s theme was, “Controversies in Pain Research.” Five of the trainees were also selected to serve as PRF-NAPS Correspondents, who provided firsthand reporting from the event, including interviews with NAPS’ Visiting Faculty members and Patient Partners, summaries of scientific sessions, and coverage on social media. Here, PRF-NAPS Correspondent Feni Kadakia, a PhD student at University of Cincinnati, Ohio, US, provides coverage of a talk by NAPS Visiting Faculty member Rajesh Khanna, New York University Pain Research Center, US.
Rajesh Khanna gave a talk at NAPS titled, “The Last of The Unplucked Gems: Targeting Nav1.7 for Chronic Pain.” You’re probably thinking, “What does ‘unplucked gems’ mean?” Khanna explained that the phrase originated from his favorite Canadian rock band, the Tragically Hip, and their song, “The Last of the Unplucked Gems!” Khanna introduced the idea that there have been “gems” for the treatment of chronic pain, but many have ultimately become failed analgesics. Throughout his talk, Khanna made the case that targeting a specific aspect of Nav1.7, a voltage-gated sodium ion channel, may be an effective way to treat chronic pain and could be considered the last “unplucked gem.”
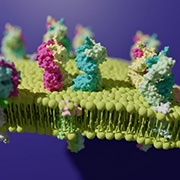
Nav1.7 is a membrane-associated channel that is highly expressed in nociceptive sensory neurons in the dorsal root ganglia (DRG) and spinal cord. Nav1.7 defines action potential threshold and contributes to its upstroke, and Khanna related Nav1.7’s function to Jimi Hendrix’s amplifier (i.e., this channel amplifies the signal so that action potentials can propagate along the neuroaxis).
Why is Nav1.7 important? About 25 years ago, humans with Nav1.7 mutations were identified, and the DRGs from these humans had excessive cellular sodium influx resulting in increased pain intensity. In contrast, other types of Nav1.7 mutations produced the opposite phenotype – congenital insensitivity to pain. These human pain syndromes produced by Nav1.7 mutations galvanized the pain field to investigate this channel, and they were genetically validated as a target for pain. So it’s no surprise that drug companies have tried to target Nav1.7 in the past; however, direct antagonism of Nav1.7 led to many clinical failures.
Why is it so difficult to target Nav1.7? Khanna provided six reasons: lack of isoform selectivity; failure to penetrate and engage spinal Nav1.7; lack of endogenous opioid system engagement; unknown state dependence of small molecule inhibitors; poor pharmacokinetic properties; and flawed clinical trial design. These led Khanna to wonder if there were alternative strategies for regulating Nav1.7 function. Perhaps blocking the channel indirectly? But how can we suppress the activity of the channel without blocking the entire channel?
Nav1.7’s protein partners
One approach would be to investigate the proteins that interact with Nav1.7. Khanna’s lab has shown that the knockdown of one such protein, CRMP2 (collapsin response mediator protein 2), reduces sodium currents through Nav1.7, suggesting that CRMP2 and Nav1.7 are functionally associated. Next, they discovered that there are modifications on CRMP2 that govern its functional regulation of other proteins. Specifically, the addition of a small ubiquitin-like modifier (SUMO), by the SUMO conjugating enzyme Ubc9 (ubiquitin-conjugating enzyme 9), controls the CRMP2 regulation of sodium currents. More simply, when CRMP2 is sumoylated, it kickstarts its regulation of Nav1.7. Moreover, when CRMP2 sumoylation is blocked, Nav1.7 currents and DRG trafficking are reduced. Such an approach (i.e., blocking CRMP2 sumoylation) can address the Nav1.7 inhibitor isoform selectivity issues and permit a reduction in Nav1.7.
This led to Khanna’s next question – can blocking CRMP2 sumoylation in vivo reverse neuropathic pain? In a model of neuropathic pain, the spared nerve injury (SNI) model, CRMP2 sumoylation is increased and drives nociceptive behaviors; however, if the injured rodents are injected with a plasmid that mimics a deficiency in CRMP2 sumoylation, painful behaviors are attenuated (Moutal et al., 2018). Moreover, Khanna’s group discovered that when they excised spinal cord and DRG tissue from these animals and performed an immunoprecipitation assay, the injured tissue expressed more sumoylated CRMP2, which could potentially serve as a biomarker.
However, can in vivo loss of CRMP2 sumoylation control Nav1.7 function? To address this, Khanna’s lab created a CRMP2 knock-in mouse line (CRMP2K374A/K374A), harboring a mutation in CRMP2 at lysine 374, which reduced the expression of sumoylated CRMP2 (hereafter referred to as CRMP2 SUMO-null mice). In these mice, Nav1.7 function and membrane localization in sensory neurons were reduced. Amazingly, these mice did not develop pain. Eliminating sumoylation of CRMP2 in these mice produced lower sodium currents, less Nav1.7 expression, less excitability, and less pain (Moutal et al., 2020).
CRMP2-Ubc9 inhibition
If you’ve been interested so far, it gets even better. Khanna asked the question, “Can we develop a small molecule that inhibits CRMP2 sumoylation to control Nav1.7 function?” He is currently working toward this goal.
In 2015, Khanna created a company – Regulonix – to understand the environment of Nav1.7 and its protein neighbors, and aims to indirectly regulate Nav1.7 activity by targeting its interacting proteins. More specifically, they are trying to prevent CRMP2 sumoylation. They’ve developed a compound, 194, that can inhibit the interaction of CRMP2 and Ubc9, thereby blocking sumoylation (Braden et al., 2021).
Importantly, 194 reduces sodium currents specifically via the Nav1.7 channel, and not other related Nav channels. The compound works across multiple species from mouse to pig to human DRGs, boosting the translational value of this compound. Its actions were independently replicated in three labs globally. Most notably, in CRMP2 SUMO-null mice, the addition of 194 had no effect on the total sodium currents recorded from DRGs, confirming 194’s mechanism of action to be via CRMP2 sumoylation.
Next, the researchers assessed how 194 influenced nociceptive behavior in injured animals. They observed that 194 can produce pain relief throughout the duration of behavioral testing and in a dose-dependent response. This pin reversing effect was seen in different pain models, including paclitaxel-, formalin-, and post-surgical pain, as well as itch. Khanna also explained that 194 can reverse and prevent oxaliplatin-induced allodynia. This is fascinating because 194 administration after injury can reduce pain, but 194 administration before oxaliplatin treatment can also prevent pain development, suggesting that this treatment could potentially alter disease progression.
While Khanna has established that 194 can reduce evoked von Frey mechanical hypersensitivity in injured mice, threshold tests are not the only measures of pain. Using the mechanical conflict avoidance system, which tests affective pain by utilizing a noxious mechanical stimulus, mice with the chronic constriction injury neuropathic pain model exhibit latencies similar to naive mice when given 194 (Li et al., 2022). Additionally, when combining 194 with low doses of gabapentin or morphine, there is a synergistic effect, implying that an added value of 194 could be its ability to lower the well-known side effects of these pain medications.
In a final question, Khanna asked, “Can the loss of CRMP2 sumoylation control Nav1.7 function through the actions of endogenous opioids?” Previous Nav1.7 blockers may have failed because they did not engage the endogenous opioid system. Khanna’s group explored this question by using mice that exhibited paclitaxel-induced mechanical hypersensitivity. These mice were administered either vehicle or naloxone (an opioid antagonist), along with 194, and the investigators observed that while mice that were administered vehicle showed less mechanical hypersensitivity (a surrogate measure of pain), the naloxone group did not exhibit analgesia. Therefore, naloxone negates the pain-relieving effect of 194, suggesting that 194 engages the endogenous opioid system.
Mechanistically “hip”
The mechanism of action and efficacy studies from Khanna and his group have been replicated and validated by the National Center for Advancing Translational Sciences at the National Institutes of Health in the US.
Khanna elegantly walked us NAPSters through his lab’s journey of taking this last “unplucked gem,” Nav1.7, understanding the mechanism and milieu of its protein interactions, and utilizing a new approach to indirectly regulate its activity, resulting in pain relief. Khanna’s talk was a hit, not just with the NAPSters, but also by the Tragically Hip, who even gave him recognition on Twitter!
Feni Kadakia is a PhD student at the University of Cincinnati, Ohio, US. You can follow her on Twitter – @KadakiaFeni.
Featured image: Membrane-bound Nav1.7. Credit – Dr. David Scott