Painful diabetic neuropathy remains a stubborn problem in many patients. While alterations in endogenous opioid signaling in the central nervous system (CNS) have been associated with this condition, both in rodent models and in people, possible contributions of opioid signaling in the peripheral nervous system have remained uncertain. A new study fills that gap in knowledge, identifying a pathway that could serve as a target to treat the pain from nerve damage that often accompanies diabetes.
The new research, from Peter Nawroth, University Hospital of Heidelberg, Germany, and colleagues, reveals a deficit of proopiomelanocortin (POMC) signaling in peripheral sensory neurons, in a mouse model of diabetic neuropathy. The loss of the antinociceptive effect of this endogenous opioid pathway was associated with degradation of μ-opioid receptors (MORs), and overexpressing POMC and MORs in sensory neurons reversed diabetic neuropathic pain in mice. The authors also provide evidence of a role for this pathway in patients.
“This paper is very important for how we understand the organism’s own ability to control pain,” said Claudia Sommer, a pain physician and researcher at the University of Würzburg, Germany. “If you can do something to increase the organism’s own ability to reduce neuropathic pain, this might be a very efficient treatment for it,” according to Sommer, who was not involved in the new work.
The study appeared in Nature Communications on January 18, 2021.
Hiding in peripheral nerves all along
The starting point of the research, first author Divija Deshpande told PRF, would turn out to be quite different from how the work would ultimately unfold.
“Our study was initially designed to investigate how immune cells interact with neurons in diabetic neuropathy. There were studies showing immune cells infiltrating nerves in diabetic patients and mice, and that immune cells release endogenous opioids. We thought that this interaction was somehow less significant in diabetic neuropathy, with respect to opioidergic signaling in the peripheral nervous system, and it could be tweaked to treat neuropathic pain,” Deshpande said. But the initial results from the authors' new work would push them in a different direction.
The authors first asked if POMC was expressed in the peripheral nervous system (PNS) under normal conditions, by performing gene expression experiments in lumbar dorsal root ganglia (DRG), sciatic nerves, and footpads from healthy adult mice. The investigators found Pomc gene expression primarily in the DRG.
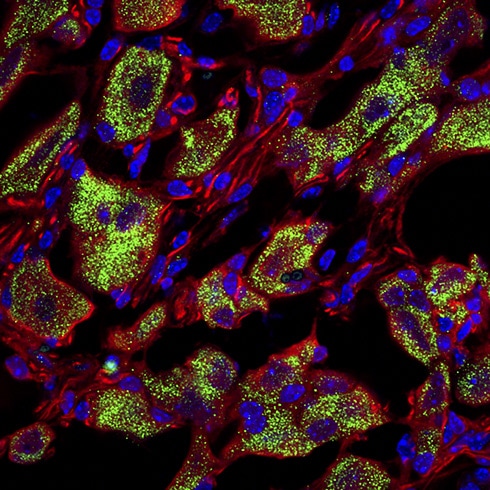
Further analysis using immunohistochemistry showed expression of POMC in DRG and in the axons of sciatic nerves. Looking at the DRG more closely, the group saw POMC expression in 60% of putative peptidergic nociceptors (marked by expression of calcitonin gene-related peptide [CGRP]), 30% of non-peptidergic nociceptors (marked by isolectin B4), and 55% of large-diameter myelinated neurons (marked by neurofilament 200). The group also saw POMC in human lumbar DRG samples.
“It was quite shocking, and it took a few months for us to get over the initial skepticism. Until now it was believed that the neurons that produced POMC were in only the CNS, but our findings showed that POMC is also expressed in the PNS,” Deshpande said.
Diabetic neuropathy dampens the peripheral endogenous opioid signaling pathway
The presence of POMC in the DRG turned the group's attention away from the immune system and toward the PNS, specifically on how the endogenous opioid system in the PNS is regulated during diabetic neuropathy.
The authors knew that POMC's antinociceptive effects in the CNS rely on the opioid pathway. Specifically, POMC is proteolytically cleaved to produce opioid peptides, which bind to opioid receptors like MORs and trigger downstream events to inhibit neuronal excitability. Deshpande had the idea that this pathway was impaired in diabetic neuropathy, leading to neuropathic pain.
To test this hypothesis, the investigators began by giving mice streptozotocin to induce diabetes. As expected, compared to untreated control animals, female mice showed hallmark signs of neuropathic pain, including increased sensitivity to mechanical von Frey hair stimuli and to heat stimuli, at 12 weeks, a time at which Pomc was downregulated in the DRG.
Moreover, MOR protein levels were also lower in the DRG of diabetic mice. This showed that the endogenous opioid pathway was depressed at both ligand and receptor levels in the PNS of diabetic mice during pain hypersensitivity.
Pomc doesn't get a promotion
What was dampening the opioidergic pathway in damaged nerves during diabetes? The authors thought that changes in Pomc transcription might be the culprit.
In silico analysis of the Pomc gene promoter revealed a region where NF-κB, an inflammatory mediator released after nerve damage, could bind. Close to this region was an area where corticotropin-releasing hormone (CRH) can bind; CRH acts as an agonist of the Pomc promoter
Deshpande thought that because the binding sites of CRH and NF-κB were in close proximity on the Pomc promoter, this suggested that if NF-κB was binding the Pomc promoter, then CRH couldn’t bind to promote POMC production.
“CRH is a fight-or-flight hormone released in the brain in extreme stress. It triggers POMC production and helps to calm down brain activity. This of course isn’t applicable in the periphery, so we were interested in CRH’s interaction with NF-κB. In our diabetic model in mice, there is nerve inflammation that triggers NF-κB activation. We wanted to see if inflammation influences POMC expression and found that POMC was lower in DRG neurons with higher NF-κB,” Deshpande said.
These findings suggested that diabetic nerve injury caused activation of NF-κB, which reduces POMC production by blocking the ability of CRH to promote Pomc transcription.
The group also observed reduced MOR in DRG neurons from diabetic mice. When cultured with high glucose concentrations, DRG neurons had high internalization of MORs, reducing their capacity to bind endogenous opioids.
Protein kinases are known to degrade MORs through phosphorylation, and the authors thought that protein kinase C (PKC) in particular could have a key role, considering that activation of this kinase is characteristic of late stages of diabetes. The researchers observed increased PKC activation in DRG neurons from diabetic mice, along with increased levels of phosphorylated MOR, which was now localized within the cells rather than on the cell membrane.
Further, a PKC inhibitor reduced MOR internalization in DRG neurons. Finally, MORs were associated with a lysosomal marker, suggesting that under hyperglycemic conditions the receptors are degraded in lysosomes.
In short, these findings showed that hyperglycemia dampened the endogenous opioid pathway in peripheral nerves by reducing Pomc transcription and increasing MOR internalization and degradation.
How does hyperglycemia set all of this into motion in the first place?
“This is the million-dollar question, and we just don't know," said co-second author Thomas Fleming. “It seems that many patients with diabetes do show increased NF-κB-mediated inflammation, but the link between hyperglycemia and neural inflammation is not exactly clear.”
Translational potential?
The team next tested if restoring endogenous POMC and MOR levels in peripheral nerves could alleviate diabetic neuropathic pain in their mouse model. To do so, they used viral techniques to overexpress POMC and/or MOR in DRG neurons in diabetic mice and measured the effects on pain behaviors.
Overexpressing POMC on its own, or with MOR, reduced neuropathic pain in male and female diabetic mice at 12 days. Specifically, this strategy reversed mechanical hypersensitivity in the animals, and a place escape/avoidance experiment showed it also reversed the aversiveness of mechanical hypersensitivity. It also rescued thermal hyperalgesia, and mice overexpressing both POMC and MOR showed even greater improvement on this measure when they also received a PKC inhibitor. Lastly, the strategy also improved non-reflexive pain behaviors, as indicated by gait analysis.
In one final experiment, showing the translational potential of the animal findings, the authors performed immunostaining of sciatic nerves from patients with type 1 and type 2 diabetes. This revealed decreased levels of POMC and MOR, compared to healthy controls.
The results suggest that targeting the peripheral POMC endogenous opioid pathway could be a potential therapeutic strategy in people with diabetic neuropathy, and other neuropathies, in the future.
“If we could target the opioid system peripherally to effectively treat neuropathic pain, that would be a big advantage. This would avoid CNS side effects of opioids, including addiction and tolerance,” Sommer said.
Exactly how best to do so remains unclear, according to Fleming.
“The problem is how to translate the idea of targeting the peripheral opioid system to treat neuropathic pain in humans,” Fleming said. "We used a viral approach to boost POMC production in DRGs in rodents, but this just isn’t possible in humans. The trick is to do this in a non-invasive way, and technologies are getting there. CRH is already used to boost POMC production in patients with Cushing's disease who have POMC deficiency, so there are ways….”
Fred Schwaller, PhD, is a freelance science writer based in Germany.